I'm in DC for the ONC Annual Meeting. Today was "invitees" only. Tomorrow is open to the public. Invitees today included the S&I Framework crowd, although most of us didn't get the message that this morning was important too. Fortunately, I got here early enough to take advantage of it.
While preparing for my flight a few weeks ago, I happened to discover that my daughter (Abby, or @amaltheafairy on twitter) was free today. So I booked her a trip for today's meeting as well. Seeing as
she was there when the ABBI project was conceived, it seemed relevant for her to hear how things were going. She'll have a report of her observations for me to post later this week. She's back at home now, ready to go back to school, after learning a ton at today's meetings. We arrived Monday night, and went to her favorite DC restaurant (
Sushi Taro). After a wonderful Omakase, she had desert combining flavors from her two favorite international destinations, France and Japan: A Green Tea Crème Brûlée. One word: Awesome.
This morning we walked from our hotel over to the meeting (about a half mile). The registration desk was such a classic representation of how these various projects communicate with each other. For each different group, there was a
very nice padded box holding printed name tags. We had registered about three weeks ago, but her tag would have been in one box (Stakeholders), and mine would have been in another (Science and Technology). I personally would have just put them all together in alphabetical order. After all, there are plenty of Beaconista's who are also involved in HIE's, and some involved in S&I Framework and so on. But for some reason, we each had a separate box. To add to the confusion, they couldn't find either of ours, so we registered again.
For the Science and Technology program, this morning's agenda was a join session between S&I Framework and the Beacon programs. I don't think anybody said anything about this to S&I Folk (but since I've been busy in the last two weeks, I can't say they didn't on one or more of the forty calls I could have been on, or the half dozen I'm usually on but didn't dial into). Last week was IHE and the mHealth Summit, so I took only a few calls that week. I heard from at least one ONC staffer (and S&I lead) that they weren't even aware of the joint session. It's a shame really, because in a room full of Beaconista's with interest in S&I Framework, there were perhaps 5 of us who were from the "volunteer pool". There were a few more than just 5 S&I volunteers present later, but most were coming for the afternoon S&I report out, or the ABBI Town Hall (which
was widely discussed in the ABBI project). If the goal of this morning's meeting (as reported by one ONC staffer) between Beacon's and S&I was to break down silos, someone at ONC should have notified all the silo owners.
We heard from two different Beacon programs first. Kicking off the program was Dr. David Kendrick, of the MyHealth Access Network. They've been doing some cool things with patient portals, and CCD documents. One of their early challenges was the quality of CCD documents being generated by Certified EHR systems. Even now, while the situation is much better, it still isn't perfect. Part of the issue seems to be with how products are installed and configured. So rather than getting the most that they are capable of, providers were barely getting the benefits. Dr. Kendrick reports having to rework a number of CCD outputs from different products. The number of products he has to deal with in his area is also rather large. He reported 30-40 products, but someone later corrected the figure to 52 separate EHR products.
One of the points that David made early on in his presentation, is that 10-20% of the effort is in the technology. The rest of the effort involves politics, policy and people issues. I've had similar experiences, where 6 months goes by to work out consent policies, and they are implemented in software in less than 6 weeks (often using
the IHE BPPC specification). And it isn't that there aren't enough standards, but rather, that more work is needed in their implementation. To quote my manager, "The trouble with standards is that there are so many to choose from."
One of the challenges still encountered is closing the referral loop: Making sure the provider making the referral gets back a report on the results of the referral. A proposed solution is to treat the referral as an order. I'm a bit challenged by that prospect, simply because I'd like to be able to make my referral choices based on quality, cost, and availability. That's information I don't have when my provider gives me a referral, and it still takes too damn long to get. I might keep my providers recommendations in mind when making my selection. IHE PCC took on a profile this year to address coordination of orders with patient documentation, which may help.
Doug Fridsma stopped by to talk to the morning group, and introduced himself as "Chief Geek" at ONC. Amusingly enough, while my current business cards say "Standards Geek", I've been seriously thinking about changing my title to "Standards Coordinator" because that seems to be what I do these days. So, I'm happy to let Doug claim the Chief Geek title. He made the point to the Beacon group that the key point in S&I was to test Health IT interventions, just as we test other interventions in healthcare.
Jim Younkin, IT Director at Geisinger Health System also harped on the CCD variation. They just rolled out a solution that allows patients to upload their own information to the portal. More than 1700 users have signed up for the patient portal there. My daughter had a great question for Jim: Can patients correct their data in KeyHIE? How does that work? I rephrased it a bit, and Jim handled the answer well, even though it wasn't what she (or I) wanted to hear. They don't have enough experience yet to know how that works. But, Jim tells us, Geisinger has had a portal for quite some time for its patients, and they've enabled patients to ask questions about their Dx, and they do, and providers handle it.
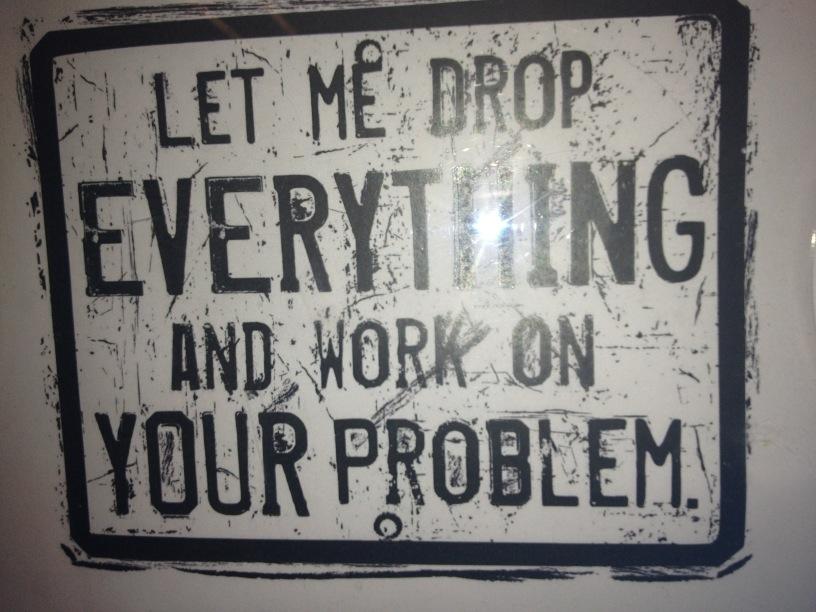
Following the Beacon presentations, we heard a QUICK review of what is going on at S&I, starting with Direct, and going through Transitions of Care, Lab Results Interface, Query Health, Provider Directories, Data Segmentation, Public Health Reporting, electronic submission of Medical Documents (esMD), Longitudinal Coordination of Care (LCC), Laboratory Ordering, and the Automate the Blue Button Initiative. There have been so many projects this year that I found this image I found at the airport tonight rather relevant:
After a little coordination from John Feikema, we slightly rearranged presentations to let Jacob head off where he needed to go. I like "Feik", but even more, I like his job. He gets to tell Doug where he needs to go, and Jacob when to stop talking.
Jacob Reider gave a pitch for Health eDecisions, and I heard from him the group's definition of CDS that happens to be the best definition I've heard ever (for CDS):
CDS is the user facing representation of clinical guidance.
Jacob then went on to describe the various components of CDS, including artifacts. What's an artifact? Basically, a CDS component you can use (like those I
describe here). E.g., a rule set, list of things to order (order set), or even a form (or template). One of the challenges in clinical guidelines (and in converting them into artifacts with actionable logic), is that you need to go beyond could/would/should and move into can/will/shall.
After Jacob was finished, we got to hear from other S&I Projects.
Abby and I tromped on down to the Workforce Development meeting to say hi to Regina Holliday, who was busy painting today. I got back upstairs in time to listen to Michael Buck's pitch for Query Health. He made several key points. One is that we need Query Health because people don't trust the government (or anyone else) to aggregate data for them. So we need to be able to send the question to the data. Another is that we have questions in New York city like "how many patients are you seeing now (a few weeks after the hurricane), vs. a month ago (before it)" that are a) Very relevant to public health, and b) aren't (and wouldn't be) addressed in any quality measure.
Today's meeting was full of TLAs, FLAs, and worse. I could barely follow the Longitudinal Coordination of Care discussions, and when CEDD came up (only the fourth acronym that thing has had), I explained it thus on twitter: CEDD = The list of things that you can ask for in Query Health.
One of the key contributions (yet to repeated well in other S&I Framework projects) was the operational workgroup in Query Health. As David mentioned earlier, technology is 20%, the rest is other stuff. The operational workgroup addressed the other stuff in Query Health, including delivering policy guidance to the 4 pilots that it is running. That's a big head start for this kind of stuff. ABBI could use a little bit of operational guidance too.
Following the S&I overviews, we broke out into four sessions. The best laid plans of ... went by the wayside. We didn't quite unconference the discussion time, but came close. I spent all my time in the Health eDecisions workgroup, and was perhaps the only volunteer present from that workgroup at a table full of Beaconista's. It's a darn shame, because I haven't been following that project nearly as well as I should. Since my daughter was next to me, I simply targeted my explanations of what we were doing to her level of understanding, and the folks at the table seemed to get what the project was doing. We had some good discussions, but not nearly as much cross-fertilization as Jacob wanted, mostly because we lacked the S&I participation. A shame, really, because a lot of great discussions could have started here.
After the discussion section, we broke for lunch. The Beaconistas headed off to a separate meeting, and we planed to resume with the S&I Round Table, and ABBI Town Hall Meetings. Abby and I went back to find Regina, took her order for lunch, grabbed nearby Chinese, and headed back to deliver Regina her lunch. We invited Regina back up to "our" room to paint during the ABBI Town Hall (Regina was there an the conception of ABBI also), and she agreed.
The S&I Round table was disappointing. Besides the fact that we'd already heard much of it in the morning (though most everyone else in the room had missed that crucial part, and thus the opportunities with the Beacon Communities), it was mostly the ONC project coordinators reporting out. I really wanted to hear from (and see) more of the S&I Community.
I must have heard the phrase "not trying to boil the ocean" three times or more. Doug must have used that phrase while putting the fear of the National Coordinator into project teams or something. The other phrase I keep hearing is "like mint.com" in reference to ABBI.
A couple of quips made it into my twitter stream while this session was going on:
- Are you a start up, or are you an up start?
- Public Health = Silos of Excellence
- LOL! This mandatory slide (slide of model) included to show relevance of informatics modeling to this problem #ONC2012
- Current speaker tells ONC that we (S&I Framework) need: Governance, governance, governance, governance, governance ... [followed by scattered applause in the room]
- A care plan is not a care plan is not a care plan. Consensus still being developed here. Rishel's law applies.
Tomorrow's post will cover the ABBI Town Hall. That was interesting enough to deserve a post of its own.